Mitral regurgitation
After aortic stenosis, mitral regurgitation is the second most common type of heart disease requiring surgery. Mitral regurgitation occurs when the atrioventricular valve between the left atrium and left ventricle of the heart is no longer able to close properly.
What is mitral regurgitation?
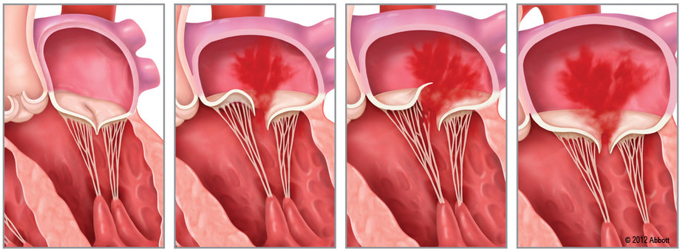
In this condition, the mitral valve, i.e. the atrioventricular valve between the left atrium and the left ventricle, becomes leaky. This leakiness results in regurgitation, with some of the blood from the left ventricle flowing back into the left atrium. Over time, this may result in the left atrium, and in severe cases even the left ventricle, becoming dilated. In addition, the fact that some of the blood constantly flows back from the left ventricle into the left atrium places excess strain on the ventricles, which may lead to heart failure.
What are the main symptoms?
Mild mitral regurgitation is common and, in many patients, does not cause any symptoms. Typical symptoms of severe heart failure are:
- Low levels of energy, fatigue
- Dyspnea upon exertion (shortness of breath)
- Skipped heartbeats or palpitations, including atrial fibrillation
What are possible causes?
Acquired mitral regurgitation can be caused by a wide variety of conditions, the most relevant of which currently include:
- Mitral regurgitation secondary to myocardial infarction
- Ischemic mitral regurgitation due to impaired blood flow to the heart muscle
- Secondary mitral regurgitation due to the dilation of the left ventricle
- Mitral valve prolapse (abnormality of the mitral valve leaflets that involves part of the leaflets protruding into the left atrium, thus preventing the mitral valve from closing properly)
- Damage to the mitral valve as a result of endocarditis
Diagnosis of mitral regurgitation
First suspicions are usually raised during a physical examination when, listening to the heart with a stethoscope (auscultation), the physician is able to detect distinctive heart sounds. Nowadays, diagnosis of mitral regurgitation is usually made using cardiac ultrasound technology (transthoracic echocardiography). Some cases may also require a further cardiac ultrasound investigation via the esophagus (transesophageal echocardiography).
Treatment for mitral regurgitation
- Medication
- Surgery
- MitraClip procedure
Medication
Heart failure medication in cases of severe mitral regurgitation with evidence of heart failure (diuretics, ACE inhibitors, beta blocker and, if appropriate digitalis or anticoagulants).
Surgery
All patients presenting with severe mitral regurgitation should be assessed in relation to possible indications for heart valve surgery. Wherever possible, valve reconstruction surgery will be performed, in order to carry out repairs on the patient's own valve.
If reconstruction surgery is not possible, the patient's valve will need to be replaced with a prosthetic valve (tissue or mechanical).
MitraClip procedure
The MitraClip procedure is a minimally-invasive, catheter-based procedure that is suitable for the treatment of severe mitral regurgitation in patients who are at high risk of complications due to concomitant disease, or are otherwise inoperable.
Where can I find out more about mitral regurgitation?
General information
Deutsche Herzstiftung (German Heart Foundation)
www.herzstiftung.de