PTCA using bare metal stents
Percutaneous transluminal coronary angioplasty (PTCA) is used to treat coronary artery stenosis. The use of bare metal stents is mainly reserved for large blood vessels, or when the patient is already receiving anticoagulants for a separate condition.

What is PTCA using bare metal stents?
A patient with coronary artery stenosis may have a stent implanted during cardiac catheterization. When compared to simple balloon angioplasty, stent treatment reduces the risk of restenosis occurring at a previously treated site. Stents may be drug-eluting or bare metal, i.e. uncoated. Not only are bare metal stents associated with quicker tissue healing, but patients receiving this type of stent also only require dual antiplatelet therapy for a duration of one month following implantation. As a result, this type of stent may be used in patients who are scheduled to undergo surgery, or in patients who are already receiving anticoagulant medication for a different condition.
Development of PTCA using bare metal stents

Stents were developed as a result of advances in the field of balloon angioplasty, and were intended to address two specific problems that can occur during or after a simple balloon angioplasty procedure.
Balloon dilation of a stenotic vessel usually results in a small tear (dissection) in the vessel wall. Although these tears are usually only partial, i.e. they only affect the inner layers of the vessel, balloon dilation can lead to parts of the inner lining coming away from the vessel wall, creating a partial or complete blockage. Prior to the introduction of stent technology, larger tears often resulted in the patient requiring emergency bypass surgery, whereas stents can now be used to support the vessel wall from the inside. This re-establishes normal blood flow and avoids the need for emergency surgery.
Another problem typically associated with balloon angioplasty is restenosis of a section previously widened using balloon angioplasty. When balloon angioplasty results in a tear forming inside a diseased vessel, this can lead to an overgrowth of scar tissue, which in turn can result in restenosis of the previously treated section (in-stent restenosis). Although the introduction of stents has helped to counteract this problem, the use of bare metal stents is associated with restenosis in 20-50% of all treated sections, with the exact rate of restenosis dependent upon the characteristics of the previously treated section (length of lesion, vessel diameter, degree of calcification).
Sigwart et al. pioneered balloon angioplasty using balloon-mounted stents, while Palmaz et al. were responsible for the development of self-expanding stents.
What conditions are treated with this procedure?
- Coronary heart disease in patients with angina pectoris
- Coronary heart disease in patients without angina pectoris, but with evidence of disturbed blood flow
What is the purpose of this procedure, and what are the results?
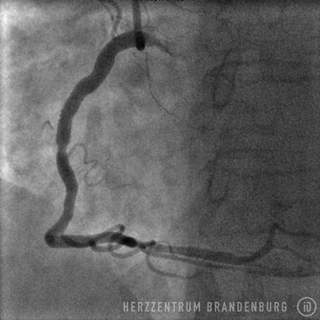
A PTCA procedure is performed in order to treat coronary artery stenosis, and to alleviate the symptoms of angina pectoris associated with physical exertion. Once the degree of narrowing reaches approximately 75%, normal blood supply is impeded during episodes of physical exertion. This leads to the heart receiving an insufficient amount of oxygen which in most patients will lead to exercise-induced chest pain known as angina pectoris. It is possible for patients with diabetes to remain asymptomatic despite clear evidence of a disruption in the normal flow of blood. This may be due to specific nerve damage typically found in patients with diabetes.
Treatment of stenosis using balloons and/or stents leads to normal blood flow being restored to a previously narrowed section. Depending on the nature of the patient's concomitant disease, and the characteristics of the stenosis, measures to prevent restenosis in the months following treatment may involve bare metal or drug-eluting stents.
Successful treatment results in significant improvements in the patient's exercise capacity, and may even lead to the patient being able to reduce the number of drugs previously required to support tissue perfusion. All patients will require long-term drug-based treatment to prevent or slow the progression of vascular disease in untreated vessels. All patients who undergo stent treatment will be required to take anticoagulant medication in order to prevent the treated vessel from becoming blocked. Patients who undergo stent treatment using bare metal stents usually only require two antiplatelet drugs (dual therapy), and only for a duration of one month.
As far as patients with clinically stable coronary heart disease are concerned, PCTA does not represent a life-prolonging solution or prevent heart attacks, except in a few very specific cases.
Treatment step-by-step
- The patient is positioned on the catheterization table, and is prepped and draped.
- After the entry site has been disinfected and numbed using a local anesthetic, a tiny incision is made in the artery.
- A guide wire is used to introduce a sheath into the artery.
- A catheter is introduced and advanced to the coronary artery.
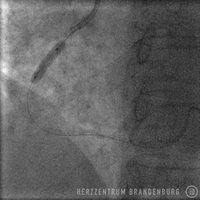
- The guide wire is used to cross the stenosis inside the coronary artery.
- The guide wire is then used to advance a stent to the site of the stenosis.
- A balloon is inflated to expand the stent.
- Balloon and catheter are removed, and the entry site is dressed with a pressure bandage, or closed using a wound closure system.
- The patient is moved to the ward for observation, and can usually be discharged the day after the procedure.
Further information
Up-to-date information on diseases of the heart and treatment options
Deutsche Herzstiftung (German Heart Foundation)
www.herzstiftung.de
Deutsche Gesellschaft für Kardiologie (German Cardiac Society)
www.dgk.org
Patientenfassung der Versorgungsleitlinie [Patient version of the treatment guidelines] www.versorgungsleitlinien.de
Sources
- Peterson KL, Nicod P (Hrsg.) Cardiac Catheterization. Methods, Diagnosis, and Therapy. 1st ed. Saunders. Philadelphia, Toronto, Montreal, Sydney, Tokyo. 1997.
- Topol EJ (Hrsg): Textbook of Interventional Cardiology. 5th ed. Saunders, Elsevier. Philadelphia 2008.
- Krakau I: Das Herzkatheterbuch. [The Book of Cardiac Catheterization] Thieme Stutgart, New York 1999.
- Julian D, Braunwald E (Hrsg): Management of acute myocardial infarction. Saunders. London, Philadelphia, Toronto, Marrickville, Tokyo 1994.