Rotablation for coronary artery stenosis
Coronary artery stenosis can occur as a result of the normal aging process in patients with exposure to a number of different risk factors. Where this process is accompanied by large amounts of calcified deposits building up inside the vessel walls, treatment is made easier and less risky if these calcified deposits are first removed using a tiny drill.

What is rotablation for coronary artery stenosis?
Rotablation represents an addition to the standard PTCAprocedure. While a standard PTCA procedure is limited to the use of balloons and stents, rotablation also uses a tiny drill, powered by compressed air, to remove calcified deposits. Rotablation is usually followed by balloon angioplasty, and the implantation of one or more stents.
What conditions are treated with this procedure?
- Coronary heart disease in patients with angina pectoris
- Coronary heart disease in patients without angina pectoris but with evidence of disturbed blood flow
Historical origins and development
In 1929, the first catheterization of a human heart took place in Eberswalde, in the Federal State of Brandenburg, and was performed by Werner Forssmann, a German urologist. At that time, and for many years to come, the procedure was limited to investigations involving the right side of the heart. During the 1950s, and after undergoing further developments, the technique finally allowed access to be extended to the left side of the heart. In 1959, Mason Sones performed the first catheterization procedure involving contrast agents, which allowed selective visualization of the coronary arteries using x-ray technology.
Over the course of the next few years, cardiac catheterization was mainly used for diagnostic purposes. It was not until the early 1970s that Andreas Grüntzig discovered that balloon catheters could be used in the treatment of stenotic blood vessels. After managing to reduce the size of the balloon catheters used, Grüntzig performed the first-ever balloon angioplasty procedure on a coronary artery in 1977.
Before the advent of stents (see separate section), the effectiveness of the angioplasty procedure was limited by the vessel's elastic recoil. Ahn et al. were the first to describe a procedure that involved a tiny drill, which was powered by compressed air and which was used to remove the material responsible for the stenosis.
Ever since the introduction of stents, which allow a controlled over-expansion of the affected blood vessel, elastic recoil no longer plays any part in chronic restenosis. Nowadays, rotablation is used in cases with severe calcifications, in cases with stenosis so severe that it can only be crossed with a wire, not a balloon, and in cases with calcifications so severe that they prevent a balloon from being inflated, even at high pressures.
What is the purpose of this type of treatment, and what are the results?
A PTCA procedure is performed in order to treat coronary artery stenosis, and to alleviate the symptoms of angina pectoris associated with physical exertion.
Rotablation can make treatment possible, or at least easier, in cases where imaging technology reveals severe calcifications, or in cases where calcifications are so severe that only a wire, not a balloon, can cross the site of stenosis.
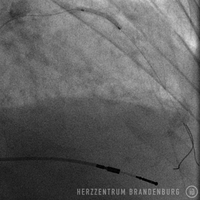
For rotablation to take place, access to the coronary artery has to be established using standard procedures (please refer to the section on PTCA). A special guide wire, which is required for the drill, is advanced past the site of stenosis. After a trial run outside the body, the guide wire is then used to advance the drill head to the site of stenosis. The drill, which is powered by compressed air, is advanced through the site of stenosis at a speed of 140,000-160,000 rpm. The process of drilling through plaque and calcified deposits inside the site of stenosis generates tiny fragments of debris, which can easily pass through the blood vessels and are absorbed by the body.
Once the drill head has been retracted, the site is widened using balloon angioplasty as per standard PTCA procedures. This step is usually followed by the implantation of drug-eluting stents (please refer to separate section), which ensure that treatment results remain satisfactory over the long term. In many cases, high pressure balloons are used to ensure that the stents are fully expanded.
By using a drill that removes calcified deposits, the operator can ensure that the stent does not get caught in calcified deposits, and is not prevented from being advanced into the target zone.
Rotablation is not suitable in cases where balloon angioplasty has resulted in tears to the vessel walls, where there is evidence of blood clots, or where there is a high degree of vessel tortuosity. As a heart attack is usually associated with blood clotting inside the blood vessels, rotablation is not usually suitable for use in patients with acute heart attack.
What happens during rotablation for coronary artery stenosis?
- Following the application of a local anesthetic, a tiny incision is made in an artery.
- A guide wire is used to introduce a sheath into the artery.
- A catheter is introduced and advanced to the coronary artery.
- The guide wire is used to cross the stenosis inside the coronary artery.
- The drill head is used to remove plaque deposits.
- The guide wire is used to advance a balloon and/or a stent to the site of the stenosis.
- The balloon is inflated and/or the stent expanded.
- Balloon and catheter are removed. A pressure bandage may be applied to the entry site, or it may be closed using a wound closure system.
- The patient is usually kept under observation for a duration of 48 hours.
Web links
Deutsche Herzstiftung (German Heart Foundation)
http://www.herzstiftung.de/
Deutsche Gesellschaft für Kardiologie (German Cardiac Society)
http://dgk.org/
Patientenfassung der Versorgungsleitlinie [Patient version of the treatment guidelines]
http://www.versorgungsleitlinien.de/patienten/khkinfo
Suggested literature on this treatment option
Tran T, Brown M, Lasala J: An evidence-based approach to the use of rotational and directional coronary atherectomy in the era of drug-eluting stents: when does it make sense? Catheter Cardiovasc Interv. 2008 Nov 1;72(5):650-62.
Sources
- Peterson KL, Nicod P (Hrsg.) Cardiac Catheterization. Methods, Diagnosis, and Therapy. 1st ed. Saunders. Philadelphia, Toronto, Montreal, Sydney, Tokyo. 1997.
- Topol EJ: Textbook of Interventional Cardiology. 5th ed. Saunders, Elsevier. Philadelphia 2008.
- Krakau I: Das Herzkatheterbuch [The Book of Cardiac Catheterization] . Thieme Stuttgart, New York 1999.
- Ahn SS, Auth D, Marcus DR, Moore WS. J Vasc Surg. 1988;7(2):292-300