Peripheral arterial disease
Peripheral arterial disease results in reduced blood flow to the limbs. The condition is characterized by an aching in the legs, which is brought on by walking. Due to the typical symptoms associated with the disease, it is commonly referred to as "smoker's leg" or "window shopper's disease" in German.
Contact
What is peripheral arterial disease?
Peripheral arterial disease (PAD) develops when atherosclerosis (hardening of the arteries) results in reduced blood flow to the legs or - less commonly - the arms. Due to the fact that this condition produces pain when walking and is commonly associated with smoking, the German language also refers to it as "smoker's leg" or "window shopper's disease". This is because people affected by the condition are forced to stop and rest at regular intervals while waiting for the pain to pass.
What are the main symptoms?
Depending on the severity of the condition, peripheral arterial disease is usually divided into four stages of severity. At stage I, the patient is still asymptomatic. As the disease progresses and the arteries become increasingly narrowed, the following symptoms may develop:
- Pain while walking, also referred to as "intermittent claudication" or limping.
- Rest pain in the lower limbs
- Gangrene and/or necrosis, e.g. in the feet
What are possible causes?
As with coronary heart disease and myocardial infarction (heart attack), peripheral arterial disease almost always occurs as a result of atherosclerosis, i.e. hardening of the artery walls. The disease tends to mainly affect the arteries in the pelvis and the legs. Important risk factors for atherosclerosis include:
- Smoking
- Diabetes
- High blood pressure
- Abnormalities in lipid metabolism
Diagnosis of peripheral arterial disease
When a patient presents with symptoms that are characteristic of peripheral arterial disease, diagnosis is usually relatively straightforward.
- Blood pressure measurements: The ankle-brachial index (ABI), a test that involves taking measurements from the arm and comparing them to measurements from the legs, can be used to quantify the degree of arterial narrowing present.
- In addition, ultrasound investigations can provide information on the extent of arterial deposits present, and on how well blood is flowing through the blood vessels.
- A type of CT or MRI scan, performed using contrast agents, allows the physician to clearly visualize the arteries.
- The catheter-based visualization of the arteries using contrast agents (angiography) is considered the gold standard in the diagnosis of PAD. This procedure allows visualization of even very small blood vessels. It is also used to guide the implantation of stents inside the narrowed sections of affected vessels.
Treatment of peripheral arterial disease
The purpose of treatment is to improve the patient's quality of life, and to halt progression of the disease in order to prevent one of its possible outcomes: amputation. Treatment can involve a number of different strategies:
- Targeting the causes of the disease
- Supervised walking program
- Medication
- Catheter-based procedures
- Vascular surgery
Targeting the causes of the disease
Avoidance of nicotine; regular physical exercise; if appropriate, control of high blood pressure and/or diabetes; lowering blood cholesterol.
Supervised walking program
This can improve blood flow in the legs by stimulating the body's natural ability to form new systems of vessels to divert the flow of blood around a blockage.
Medication
Patients may also benefit from certain medications. Substances such as acetylsalicylic acid, more commonly known as aspirin, can improve blood flow.
Catheter-based procedures
Via a small incision in one of the arteries in the groin, the physician advances an inflatable balloon catheter to the narrowed section of the affected artery. Once the narrowed section has been widened by inflating the balloon, a stent is inserted to support the vessel walls. This method is particularly effective when dealing with shorter sections of narrowing inside arteries.
Vascular surgery
In some patients, it may be possible to surgically remove arterial deposits from the arteries in the upper thigh. Depending on the location of the blockage, bypass surgery may be possible. For this procedure, the physician uses either one of the patient's own veins or a synthetic blood vessel made of teflon in order to create a bypass around the narrowed artery.
Peripheral arterial disease
When fatty deposits (atherosclerosis) are laid down inside arteries as a result of diabetes, high blood pressure, smoking, obesity or genetic factors, this may result in narrowing (stenosis) of the blood vessels. While stenosis can develop anywhere, the condition has a tendency to manifest at specific sites. Sites often affected by stenosis include the coronary arteries (coronary heart disease, CHD), the carotid arteries, the renal arteries, as well as the arteries of the pelvis and lower limbs. Stenosis of the arteries that run through the arms is less common, and usually affects the point where subclavian artery arises from the aorta.
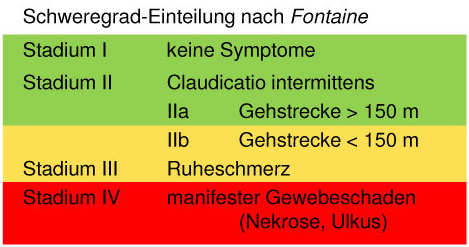
At a degree of stenosis exceeding 50% of the vessel's diameter, the patient will develop symptoms associated with poor blood flow. Stenosis affecting the carotid artery is a sub-type of this condition with very specific characteristics, and is dealt with in a separate section. When the peripheral arteries, and in particular the arteries of the pelvis and the legs, are affected by reduced blood flow, symptoms associated with this reduced blood flow usually develop as a result of physical activity. This is because the skeletal muscles require more oxygen during periods of physical activity than during periods of rest. Lack of oxygen (ischemia) leads to the build-up of lactic acid, which in turn causes pain. Clinical symptoms are commonly divided into four stages of severity, based on the degree of narrowing present. This type of classification can help assess individual patients in terms of their diagnostic and treatment requirements. Symptoms are classified according to Fontaine (Fig. 1).
- Fontaine stage I: While there is some narrowing present, the patient is asymptomatic.
- Fontaine stage IIa: There is a degree of claudication (usually affecting the legs; intermittent claudication: "window shopper's disease"). The patient can walk more than 200 meters without developing pain or having to stop and rest.
- Fontaine stage IIb: The patient can walk less than 200 meters before developing pain.
- Fontaine stage III: Pain develops even after a very short walk or at rest.
- Fontaine stage IV: Reduced blood flow has started to cause tissue death (gangrene), which usually affects the foot (in particular the toes).
No immediate action is required during stages I and IIa. In contrast to coronary heart disease, PAD does not necessarily place patients at immediate risk of life-threatening events such as a heart attack. Patients are advised to follow a program of walking. In combination with medication to improve blood flow through the arteries (e.g. platelet aggregation inhibitors, which prevent platelet adhesion, thus improving blood flow in smaller blood vessels), this can stimulate the body's natural ability to form new blood vessels (neoangiogenesis). The effect is, however, limited. Patients with PAD Fontaine stage IIb or above should undergo further diagnostic testing.
Diagnosis
- Blood pressure measurements: A comparison of blood pressure measurements from the legs and the arms (ankle-brachial index) can help pinpoint the location of the stenosis (narrowing).
- Ultrasound scan: in addition to the above, an ultrasound scan can show stenotic areas, arterial deposits, and the flow of blood through the blood vessels.
- CT, MRI: computed tomography (CT) and magnetic resonance imaging (MRI) are excellent tools for visualizing the major blood vessels of the body.
- Angiography: this catheter-based technique, which uses dyes to make the blood vessels visible, remains the gold standard in diagnostic techniques. This is because it allows the physician to identify the exact location, as well as the severity, of areas of stenosis in any of the body's blood vessels, including the very small ones. Furthermore, this technique allows treatment to be initiated immediately, as part of the same procedure. As long as the affected vessel is easy to reach with a catheter, the physician can insert a stent to support the vessel walls.
Treatment for PAD by region (Fig. 2)
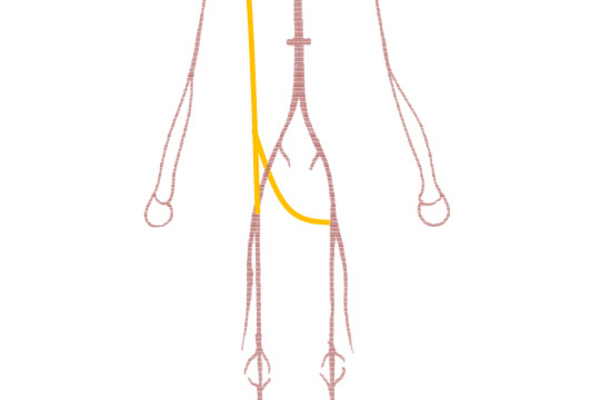
- Arm: prosthetic bypass graft from the carotid artery to the subclavian artery (in the arm) beyond the point of stenosis (carotid-subclavian bypass; carotid-axillary bypass) (Fig. 3).
- Pelvis: Y-shaped artificial prosthetic graft from the aorta to the iliac or femoral arteries (aorto-biiliac bypass, aorto-bifemoral bypass), or a one-sided bypass graft, using a straight artificial prosthetic graft from the aorta to the iliac artery (aorto-iliac bypass), or to the femoral artery (aorto-femoral bypass) (Fig. 3).
- Legs: groin - endarterectomy and patch angioplasty (Fig. 4)
- Thighs: femoro-popliteal I bypass using prosthetic graft (from femoral artery to popliteal artery above the knee) (Fig. 5).
- Calves: femoro-popliteal III bypass (from femoral artery to popliteal artery below the knee) using a vein graft or a combination of vein and prosthesis if only an insufficient length of vein is available (prosthesis above the knee, with vein graft reaching from there to beyond the knee: this is known as a composite graft) (Fig. 5). If only an insufficient length of vein is available, the bypass is performed using prostheses made from special kink-resistant material (known as ringed grafts)
- Lower calves: femoro-crural bypass (from the femoral artery to one or several arteries in the lower calf) (Fig. 6).
- Foot: from the femoral artery or the popliteal artery to one of the two pedal (foot) arteries (femoro-pedal bypass; popliteal-pedal bypass) (Fig. 6).
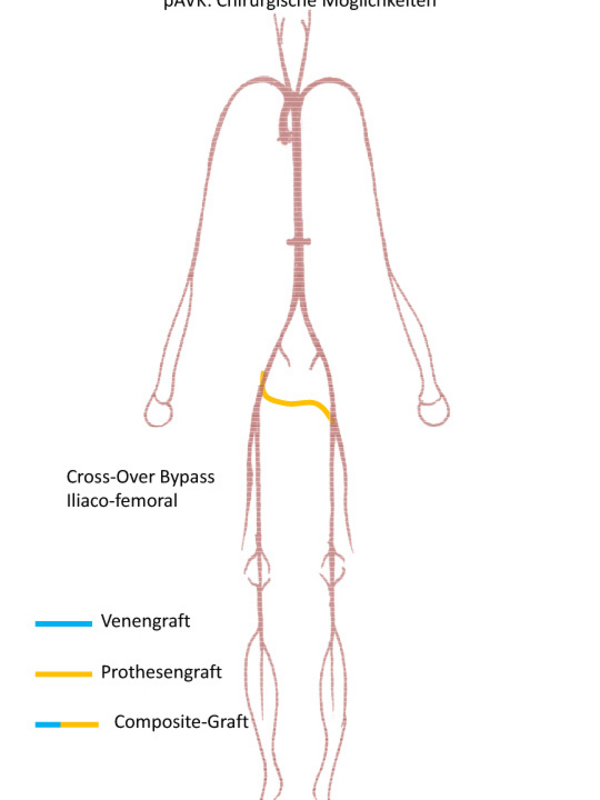
Specialist procedures in complex cases with stenosis (narrowing) affecting arteries at different levels:
Extra-anatomic bypass procedures: from the artery in the arm to one or both of the femoral arteries (axillo-femoral or axillo-bifemoral bypass) (Fig. 7). Crossover bypass from the iliac artery (pelvis) or the femoral artery on one side of the body to the femoral artery on the contralateral side (iliaco-femoral crossover bypass; femoro-femoral crossover bypass) (Fig. 8).