Cardiovascular magnetic resonance imaging (cardiac MRI)
Cardiac MRI is one of the most important non-invasive diagnostic techniques available. A cardiac MRI does not only provide a clear insight into the processes taking place inside the heart, but can also be used to help differentiate between different types of tissues, as well as allowing an assessment of heart function.
Contact
What is meant by cardiovascular magnetic resonance imaging (cardiac MRI)?
Cardiac MRI uses strong magnetic fields and specific radiofrequency pulses that excite molecules inside the patient's body (mainly hydrogen atoms), causing them to emit energy. This energy is then measured and converted into a digital signal, which is used to produce an image.
The main advantage of this technology is that it does not require ionizing radiation or iodine-based contrast media. A cardiac MRI usually takes between 45-60 minutes. Aside from using ECG triggering, the technology also requires the patient to hold their breath at certain stages during the process. Depending on the type of condition involved, cardiac MRI investigations may require contrast agents (gadolinium) to be injected via a peripheral IV access.
Possible applications
Coronary heart disease
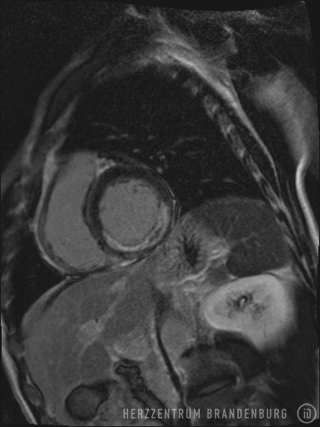
- Assessment of cardiac vitality (see Fig. 1: Visualization of scarring following myocardial infarction)
- Evaluation of myocardial ischemia (adenosine/dobutamine stress MRI)
While cardiac MRI does not currently have a role in the assessment of coronary stenosis, it is sometimes used in the diagnosis of congenital vascular malformations.
Congenital heart defects
- Morphology
- Assessment of the severity of cardiac shunting
- Monitoring of patient progress following corrective surgery (due to the nature of our patient pool this is a very rare indication)