Atrial septal defect repair
It is necessary for an atrial septal defect to be repaired if it involves a hole in the septum, i.e. the wall between the two atria. While patients with this type of defect used to require open heart surgery, they can now be treated using catheter-based techniques and special occlusion systems.
Contact
What is percutaneous repair of an atrial septal defect?
Percutaneous repair of an atrial septal defect is a catheter-based procedure to close a hole in the atrial septum (using a closure device called an ASD or PFO occluder).
The procedure is used to repair an atrial septal defect. This type of defect is usually congenital, and is characterized by a hole in the septum between the left and right atria. In some cases, this type of defect may also be caused by the incomplete closure of the foramen ovale, a condition known as a patent foramen ovale. In certain situations, this type of defect may lead to a venous thrombus crossing the foramen ovale and causing a stroke, e.g. when scuba diving. When the atrial septal defect reaches a certain size, the patient is at risk of heart failure. All of the above cases require the atrial septal defect to be repaired. While in the past, patients with an atrial septal defect had to undergo open heart surgery, many patients can now be treated using catheter-based techniques and special occlusion systems, which are referred to as occluders or septal umbrellas.
The origins of percutaneous repair
Ever since the first percutaneous repair of an atrial septal defect was described in 1974, a number of different occlusion systems have been developed. The procedure has since become an established part of routine clinical practice.
When should percutaneous repair be used?
- Symptomatic patients with patent foramen ovale (PFO) and stroke
- Larger atrial septal defects (ASD)
How can percutaneous repair help?
Percutaneous repair is a catheter-based procedure that uses special occluders to close an atrial septal defect. This prevents blood and thrombi from crossing the hole in the wall between the two atria. Most occluders consist of a flexible nitinol wire mesh, which becomes gradually covered by endocardium during the healing process.

A step-by-step description of percutaneous repair
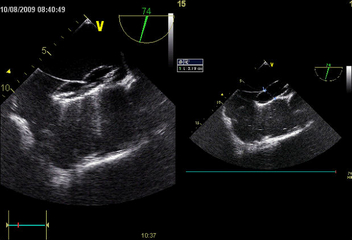
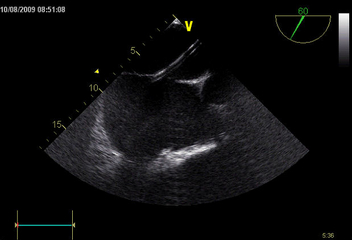
Certain anatomical conditions have to be met if an occluder device is to be used. As a result, in order to decide whether a catheter-based procedure is possible, our hospital requires patients to undergo transesophageal electrocardiography as part of essential pre-operative testing.
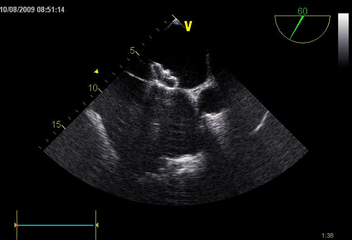
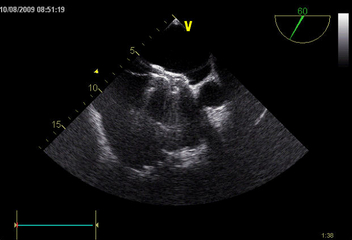
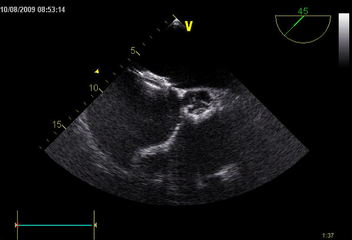
- The procedure takes place in our catheterization laboratory, and is performed using local anesthesia. Transesophageal echocardiography (a cardiac ultrasound performed via the esophagus) is used to guide the positioning of the occluder device. Implantation of the umbrella device is therefore performed under a form of anesthesia that is mild enough to ensure that the patient is asleep, while also ensuring that breathing and circulation remain stable.
- Once a small incision has been made in one of the large veins in the groin, a wire is positioned in such a way as to reach through the atrial septal defect and into one of the pulmonary veins. The wire is then used to advance a sheath 3-4 mm in size from the groin into the left atrium. This sheath is used to position the occluder device inside the atrial septal defect or patent foramen ovale. Once the occluder system has been positioned correctly, it is detached from the introducer set.