
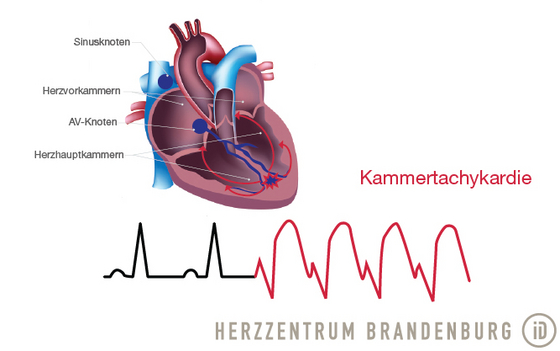
Ablation of ventricular tachycardia (VT)
Ventricular tachycardia is a type of recurrent, malignant arrhythmia that originates in one of the ventricles of the heart. This type of arrhythmia may benefit from catheter ablation.
Contact
What is ventricular tachycardia?
Ventricular tachycardia is a type of life-threatening arrhythmia affecting the ventricles, which places the patient at risk of sudden cardiac death. When a patient is diagnosed with ventricular tachycardia, the treatment of choice usually includes the implantation of an ICD (implantable cardioverter defibrillator) for the secondary prevention of sudden cardiac death.
Some cases of a specific type of VT referred to as monomorphic ventricular tachycardia, which has a regular pattern of occurrence and always originates from the same area of the heart, may also be treatable using catheter ablation. Prior to commencing treatment, it is necessary to establish whether the patient has any underlying heart disease. Sometimes, treatment of an underlying condition will also have a positive impact on the patient's arrhythmia.
Catheter ablation of this type of arrhythmia usually requires what is referred to as 3D mapping technology. This allows 3D images to be created of the right and/or left ventricle(s), thus capturing the exact process of electrical stimulation that occurs during the arrhythmia. If the mechanism behind the tachycardia is identified, radiofrequency ablation can be used to prevent further tachycardic episodes from developing.
Very rarely, a patient may present with idiopathic ventricular tachycardia, a type of VT that occurs in the absence of other heart disease, and which usually responds well to catheter ablation.
What types of ventricular tachycardia should be treated with ablation?
A patient can be considered for catheter ablation if - despite antiarrhythmic drug therapy - they have a recurrence of ventricular tachycardia.
A step-by-step description of catheter ablation for ventricular tachycardia
If a patient has recurrent episodes of ventricular tachycardia despite antiarrhythmic drug therapy, catheter ablation can be considered.
Prior to the procedure
The examination takes place in a specially-equipped catheterization laboratory - our electrophysiology laboratory. Prior to undergoing the actual procedure, you will be connected to a number of different monitors (e.g. ECG). This allows continuous monitoring of heart function throughout the procedure.
During the procedure
At the start of the procedure, a local anesthetic is used to numb the area around the entry site(s), which is (are) usually on the right side of the groin. Electrophysiology catheters (thin, flexible probes) are introduced into the blood vessels and advanced to the heart. These catheters can record ECG readings from the inside of the heart, and are positioned using x-ray guidance.
We will usually try to trigger your arrhythmia by using imperceptible electrical impulses. This is done in order to establish whether the arrhythmia originates from inside the left or the right ventricle.
Catheter ablation usually requires what is referred to as 3D mapping technology (EnSite NavX). This allows 3D images to be created, showing the exact anatomy of the right and/or left ventricle(s) and capturing the exact process of electrical stimulation that occurs during the arrhythmia. If the mechanism behind the tachycardia can be identified in this manner, radiofrequency ablation can commence.
Once the relevant area has been successfully ablated, the procedure is often interrupted for a considerable period of time, in order to determine whether the ablated tissue is likely to recover. At the end of the procedure, the catheters are removed.
After the procedure
You will remain in the catheterization laboratory while a pressure bandage is applied to the access site. This will need to remain in place for a number of hours (exact duration to be determined after the procedure), which means you will be required to stay in bed. You will usually be able to eat and drink as soon as you are back on the ward. In rare cases, it may be necessary to monitor the patient's heart rate for some time after the end of the procedure.
Discharge from hospital
It is usually possible for patients to be discharged only a day or two after the procedure.
At home
After being discharged, you should try to avoid physical activity for a duration of one week.
Where can I find out more about ventricular tachycardia?
Deutsche Herzstiftung e.V. (German Heart Foundation)
Palpitations (racing heart)
herzstiftung.de
Deutsche Gesellschaft für Kardiologie (German Cardiac Society)
dgk.org
Deutsche Gesellschaft für Kardiologie (German Cardiac Society)
Pocket-Leitlinien Invasive elektro-physiologische Diagnostik, Katheterablation [pocket guidelines on diagnostic invasive electrophysiology, catheter ablation].
dgk.org
