Atrial fibrillation
Atrial fibrillation is one of the most common cardiac arrhythmias, and its prevalence increases with age. The condition affects 2-4% of the population aged over 60 years.
Contact
What is atrial fibrillation?
Atrial fibrillation is a type of cardiac arrhythmia. The condition is characterized by an abnormal heart rhythm that originates in the atria and is propagated in a circular pattern. From the atria, the impulses are transmitted to the ventricles, and produce a change in the heart rate depending on whether this occurs at a slow (bradycardia) or a fast rate (tachycardia). Atrial fibrillation can be present long-term (permanent), or it may be experienced as recurring episodes (paroxysmal). The condition is always associated with an irregular heartbeat, which is therefore its cardinal symptom. While not dangerous in itself, some patients may experience the symptoms associated with the condition as extremely uncomfortable. Symptoms, however, vary greatly from one patient to another, with some patients experiencing no symptoms at all.
![[Translate to Englisch:] Abbildung Absolute Arrythmie - Immanuel Herzzentrum Brandenburg in Bernau bei Berlin [Translate to Englisch:] Abbildung Absolute Arrythmie - Immanuel Herzzentrum Brandenburg in Bernau bei Berlin](/assets/_processed_/8/8/csm_immanuel-herzzentrum-brandenburg-in-bernau-bei-berlin-vorhofflimmern_dd81f1e009.jpg)
The main complication of the condition is stroke, which may occur as a result of blood clots travelling to the brain from the left atrium.
During atrial fibrillation, the atria can no longer pump blood effectively. The result is reduced flow velocity, which increases the chance of blood clots forming, particularly in the left atrium. If these blood clots leave the left atrium, the risk of embolisms increases. The risk of stroke is particularly high, but there is also an increased risk of embolisms affecting organs in the rest of the body. Following an initial risk assessment, most patients with atrial fibrillation will need to start anticoagulant medication to prevent blood clots from forming. Aside from traditional, oral anticoagulants (blood thinning medication), treatment may include new drugs such as Falithrom /Marcumar [phenprocoumon] and, in rare cases, even drugs such as Dabigatran and Rivaroxaban, both of which are members of a new generation of blood thinning drugs.
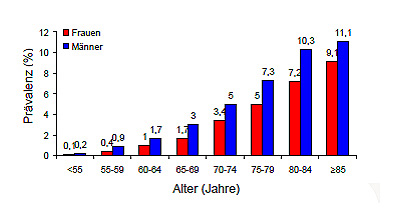
Prevalence (frequency) of atrial fibrillation, ATRIA study, USA
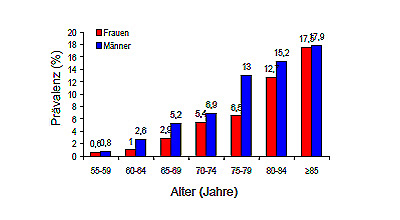
Prevalence of atrial fibrillation, Rotterdam study, Europe
What are the main symptoms?
Patients usually experience atrial fibrillation as irregular palpitations. However, results from a number of in-depth investigations show that many patients remain unaware of both shorter and longer episodes of atrial fibrillation.
- Palpitations / skipped beats
- Reduced exercise capacity
- Dyspnea (shortness of breath)
- Dizziness
- Anxiety
- Frequent urination
- Frequently remains unnoticed
What are possible causes?
Atrial fibrillation can usually be traced back to an underlying heart condition such as heart valve disease, coronary heart disease or heart failure, but also high blood pressure, or thyroid disorders. In 15% of cases, however, the cause remains unknown.
Treatment for atrial fibrillation
With regard to treatment, there are two different approaches, one aimed at reducing the heart rate, the other aimed at restoring regular sinus rhythm.
- Rate control using, e.g. beta blockers, Verapamil, Digitalis
- Restoration of sinus rhythm (cardioversion) using either medication such as, e.g. Amiodarone, Felcainide, or electric cardioversion
- If the patient's atrial fibrillation has been ongoing for some time, or if the initial onset of the condition is unknown, where appropriate, transesophageal echocardiography may be used in order to exclude the presence of blood clots inside the left atrium.
- Electrophysiology procedures with isolation of the pulmonary vein (in patients with recurrent symptomatic atrial fibrillation that have not responded to drug therapy)
- Oral anticoagulants to reduce blood clotting and prevent stroke
Where can I find out more about atrial fibrillation?
General information
Deutsche Herzstiftung e.V. (German Heart Foundation)
www.herzstiftung.de
Information specifically on atrial fibrillation
Kompetenznetz Vorhofflimmern (The German Competence Network on Atrial Fibrillation, AFNET)
www.kompetenznetz-vorhofflimmern.de
